Philanthropy and donations
The Centre for Online Health has made a significant impact on the lives of Australians by using telehealth and virtual care to improve access to health services. For more than two decades, our research achievements have relied upon competitive research grants, the support of industry partners, and the generosity of donors and philanthropists.
If you would like to support our work, we would welcome the opportunity to share our ideas and hear more about your personal interests and passion. Your generosity will continue to make a difference in the way healthcare is made available in a fair, convenient and equitable manner.
Philanthropic supporters have the potential to make a significant difference in furthering our research which really makes a difference.
For further information regarding our projects, donations and philanthropy – please contact:
- Professor Anthony Smith
Director, Centre for Online Health
E: asmith@uq.edu.au
W: https://coh.centre.uq.edu.au
- Jo Cherriman
Senior Manager, Advancement and Development
E: j.cherriman@uq.edu.au
W: Advancement - Faculty of Medicine - University of Queensland (uq.edu.au)
Here are some UQ Centre for Online Health project opportunities:
Using telehealth to provide better access to services
The delivery of care by telehealth usually involves support by telephone, videoconference or by remote patient monitoring. It was once thought that telehealth was designed only for people living in very remote areas, but in fact telehealth can help everybody. During the pandemic, telehealth became a household name as general practitioners moved many of their services to include virtual care. Led by Professor Anthony Smith, the Centre for Online Health (COH) is best known for its practical research and service programs which involve:
- Engagement with community, patients, and service providers;
- Identification of health priorities and preferences; and
- Creation of innovative ways to make services more easily accessible and sustainable.
Our work to date has demonstrated some remarkable benefits including earlier detection of chronic disease, more convenient access to healthcare, new models of care which are more tailored to patient needs, and direct savings to families due to reduced travel away from home.
Chronic disease care using telehealth
The problem: One in five Australians have more than one chronic health condition (e.g., diabetes, asthma, back pain, heart disease, etc.). The healthcare system is failing to give people the care they need because it is designed to treat one condition at a time. And costs are growing, with the average healthcare spend per capita increasing by 6.6% in 2020-21. One in eight Australians with multiple chronic conditions have experienced issues because the communication between their healthcare professionals is poor. Previous research identified that care that not only asks for but takes into account people’s opinions, is clearly communicated between health professionals and takes advantage of existing technologies can lead to better outcomes and quality of life for people with multiple health conditions.
The solution: Using a consumer-led approach, we want to integrate safe and effective health technologies (e.g., mobile apps, telehealth, etc) to provide consistent and personalised support for people to self-manage their own conditions. Existing technologies (e.g., clinical dashboards, eConsults) will also be used to facilitate the communication and integration of the work done by multiple healthcare professionals, increasing the capacity of health teams to care for people with chronic conditions. This work will be conducted at The University of Queensland Centre for Online Health, globally recognised with more than 20 years
Class-e-Care for Kids
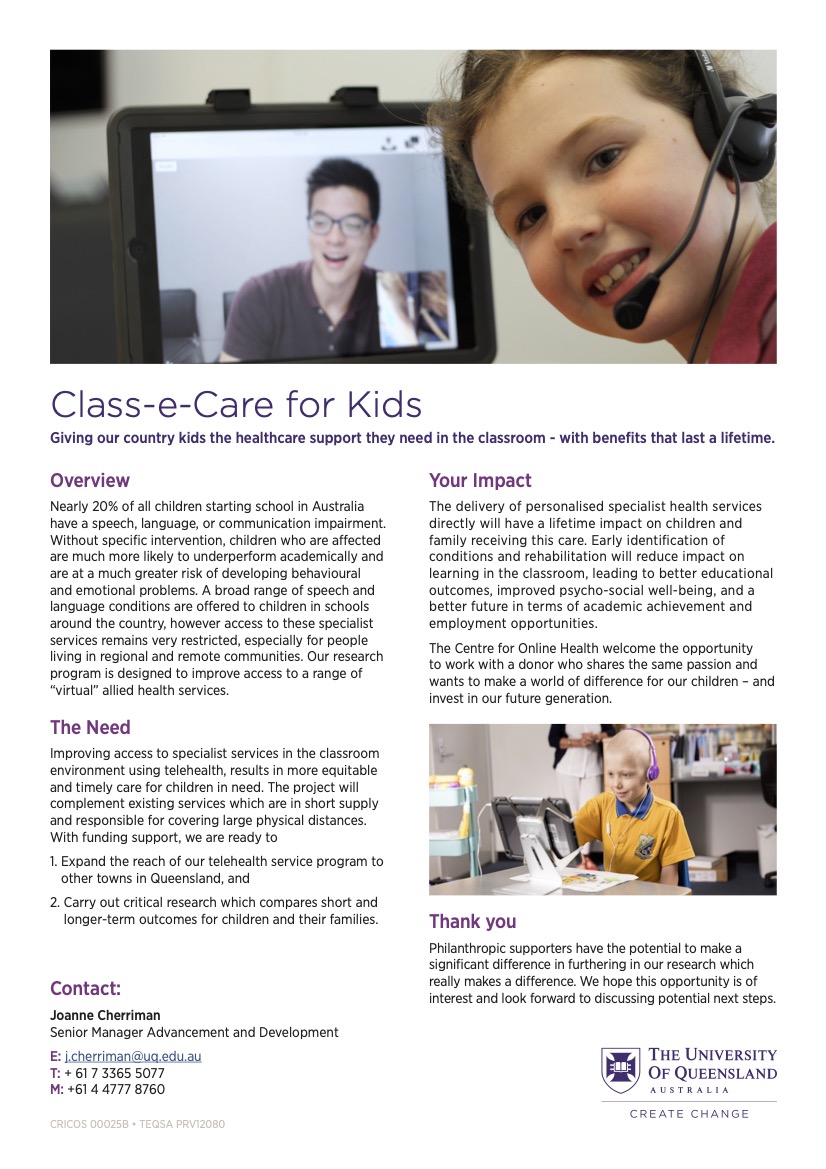
Nearly 20% of all children starting school in Australia have a speech, language, or communication impairment. Without specific intervention, children who are affected are much more likely to underperform academically and are at a much greater risk of developing behavioural and emotional problems. A broad range of speech and language conditions are offered to children in schools around the country, however access to these specialist services remains very restricted, especially for people living in regional and remote communities. Our research program is designed to improve access to a range of “virtual” allied health services.
LLMs and Telehealth (such as ChatGPT)
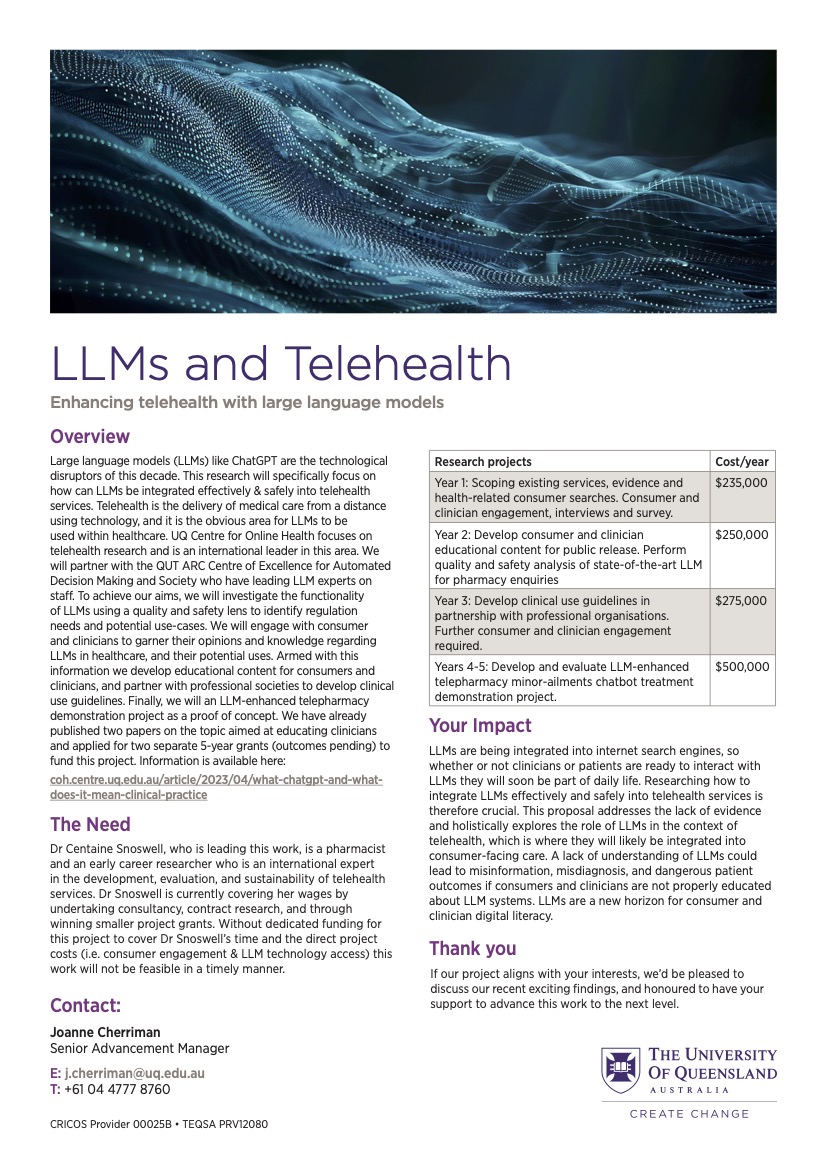
Large language models (LLMs) like ChatGPT are the technological disruptors of this decade. This research will specifically focus on how can LLMs be integrated effectively & safely into telehealth services. Telehealth is the delivery of medical care from a distance using technology, and it is the obvious area for LLMs to be used within healthcare. UQ Centre for Online Health focuses on telehealth research and is an international leader in this area. We will partner with the QUT ARC Centre of Excellence for Automated Decision Making and Society who have leading LLM experts on staff. To achieve our aims, we will investigate the functionality of LLMs using a quality and safety lens to identify regulation needs and potential use-cases. We will engage with consumer and clinicians to garner their opinions and knowledge regarding LLMs in healthcare, and their potential uses. Armed with this information we develop educational content for consumers and clinicians, and partner with professional societies to develop clinical use guidelines. Finally, we will an LLM-enhanced telepharmacy demonstration project as a proof of concept. We have already published two papers on the topic aimed at educating clinicians and applied for two separate 5-year grants (outcomes pending) to fund this project. Information is available here: coh.centre.uq.edu.au/article/2023/04/what-chatgpt-and-what-does-it-mean-clinical-practice
Telepalliative Care
Palliative care provides physical, psychological and spiritual support for people with a terminal illness. Increasing the likelihood of a “good death”, palliative care is incredibly important for improved: quality of life; pain relief; care closer to home and; bereavement outcomes for family. For instance, 70% of Australians prefer to die at home but only 14% actually do. Palliative care assists people to die in their place of choice.
However, with 84% of palliative care teams being in major cities, palliative care access decreases with increasing remoteness. Telehealth (especially videoconsultations and remote patient monitoring) allows palliative care teams to virtually reach into people’s homes to provide support. The value of telehealth in increasing access to palliative care, for people with a terminal illness and their families, cannot be understated. Yet, in Australia, and globally, the challenge remains regarding how best to make telehealth a routine part of healthcare systems. The benefits of telepalliative care are substantial, but implementation can be complex.
This research will:
- Expand Palliative Care ECHO to allow more health professionals to join and interact. Palliative Care ECHO is a virtual mentoring program upskilling health professionals across Australia (especially in rural and remote) through monthly applied-teaching sessions with palliative care specialists;
- Leveraging off national partnerships, develop a website that maps services and provides information and resources for patients, caregivers and health professionals;
- Implement and evaluate telepalliative care services where needed.
Trust in Digital Health Care
Trust is intimately linked with the uncertainty of the future. Digital health (i.e. technology used to collect, store, communicate and manage health care) has been in use for over 10 years but only now are we experiencing the disruption to the way we usually receive care. This has unveiled a multitude of issues, namely:
- Prior to the COVID-19 pandemic, 60% of health professionals had never used digital health.
- Health service providers were the top source of databreaches in Australia in 2022.
- Recent estimates suggest 9 in 10 Australians do not trust digital health in some way.
Our group have been working closely with consumers for the last 3 years and we know that their trust varies amongst different virtual care modalities, being significantly impacted by positive experiences. Trust is also a predictor of digital health use, adoption, usefulness and acceptance.
It is not surprising that trust will be one of the biggest threats to delivering effective, safe, and sustainable digital health care over the next 10 years.
We strongly believe that failure to address these gaps will result in a lost opportunity in our history, where digital health models of care will be of little value to people if they cannot trust them, or if they lack the skills to effectively engage with them. The time to address this is now to ensure an equitable, sustainable, flexible, and efficient healthcare system making the most of the benefits that digital health can provide.
Examination of clinician and consumer perspectives on the use of telehealth to access voluntary assisted dying support
Voluntary Assisted Dying (VAD) is now available in all Australian states. VAD is a service that permits an eligible person with a terminal illness to end their life through self-administration or practitioner-administration of medication. Although VAD is now legal in all Australian states, the laws are unclear about whether VAD consultations can be provided using telehealth. While the current laws have not been tested in a court of law, it may currently be a criminal offense for clinicians to provide VAD advice through telehealth. Telehealth, the delivery of healthcare from a distance using technology, is used internationally to ensure that individuals, regardless of location, can access consultations and support for VAD services. VAD enables “people who are suffering and dying to choose the manner and timing of their death”. Choice is a central tenet of VAD, yet people living in regional, rural and remote (RRR) locations lack choice if local health services are not providers. Telehealth has the potential to remove these barriers and improve access to VAD information and care for individuals who need it. This research will investigate the impact of using (or not using) telehealth to access VAD services from the perspective of both consumers and clinicians in the Australian context. Funding research regarding the use of telehealth in the VAD space will improve end-of-life care for all Australians, regardless of their location.
